NEWS
View AllMarketCentral App for MSMEs
April 17, 2024ITES SMBXL, a leading technology company that supports MSMEs, launched the MarketCentral App, which has been designed using feedback received...
NATO dilemma
April 17, 2024Delimitation of LS constituencies threat to TN : Stalin
April 17, 2024E-Book
2023 ஆம் ஆண்டின் சாதனை பெண்கள்
MarketCentral App for MSMEs
April 17, 2024
NATO dilemma
April 17, 2024
Delimitation of LS constituencies threat to TN : Stalin
April 17, 2024
TASMAC closed for 3 days in TN
April 17, 2024
Beware, MacOS Ventura update is full of bugs
April 17, 2024
Seoul plans AI safety summit in May
April 17, 2024
World IT Show 2024 begins in Seoul
April 17, 2024
Revolutionizing democratic processes, AI way
April 17, 2024
Best 14-inch laptops
April 17, 2024
ISRO develops light weight rocket engines
April 17, 2024
5 IS militants in Iraq killed in air strikes
April 17, 2024
Buttler aces Narine’s ton, helps RR beat KKR
April 17, 2024
Spinner Derek Underwood passes away
April 17, 2024
Sunrisers six flurry sinks RCB in their courtyard
April 16, 2024
Mohun Bagan SG overcome Mumbai FC to lift League Shield
April 16, 2024

MarketCentral App for MSMEs
April 17, 2024
NATO dilemma
April 17, 2024
Delimitation of LS constituencies threat to TN : Stalin
April 17, 2024
TASMAC closed for 3 days in TN
April 17, 2024
Beware, MacOS Ventura update is full of bugs
April 17, 2024
Seoul plans AI safety summit in May
April 17, 2024
World IT Show 2024 begins in Seoul
April 17, 2024
Revolutionizing democratic processes, AI way
April 17, 2024
Best 14-inch laptops
April 17, 2024
ISRO develops light weight rocket engines
April 17, 2024
5 IS militants in Iraq killed in air strikes
April 17, 2024
Buttler aces Narine’s ton, helps RR beat KKR
April 17, 2024
Spinner Derek Underwood passes away
April 17, 2024
Sunrisers six flurry sinks RCB in their courtyard
April 16, 2024
Mohun Bagan SG overcome Mumbai FC to lift League Shield
April 16, 2024
Cinema
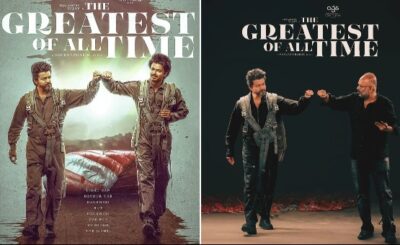
View AllVijay lends voice for ‘The G.O.A.T’ first single
April 14, 2024Chennai, Apr 14:The makers of Vijay's 'The Greatest Of All Time' announced...
STR goes for look change in ‘Thug Life’
April 14, 2024Spine-chilling teaser of ‘Sabdham’
April 14, 2024Sports
View AllButtler aces Narine’s ton, helps RR beat KKR
April 17, 2024Kolkata, Apr 17: Jos Buttler swung his bat merrily on way to...
Spinner Derek Underwood passes away
April 17, 2024
#slider > figure >a > img:hover {
-ms-transform: scale(1.5); /* IE 9 */
-webkit-transform: scale(1.5); /* Safari 3-8 */
transform: scale(1.1);
}
@keyframes slidy {
0% { left: 0%; }
20% { left: 0%; }
35% { left: -100%; }
45% { left: -100%; }
75% { left: -200%; }
85% { left: -200%; }
100% { left: -200%; }
}
body { margin: 0; }
div#slider { overflow: hidden; }
div#slider figure img { width: 20%; float: left; }
div#slider figure {
position: relative;
width: 500%;
margin: 0;
left: 0;
text-align: left;
font-size: 0;
animation: 10s slidy infinite;
}
Articles
View AllGathering storm before the ballot battle
April 14, 2024Middle East turmoil escalates as Iran pounds Israel
April 14, 2024Unforgettable politics based Tamil movies
April 14, 2024Tourism
View AllVaranasi sees boom in spiritual tourism
April 14, 2024Varanasi, Apr 14:The city of Varanasi is renowned for its sacred Ganga river, majestic ghats,...
No more smelly trains!!
April 14, 2024Chennai, Apr 14:Indian Railways is exploring new technologies and solutions to tackle...
Fun Facts!! AI imagines summer in ‘Parallel Universe’
April 14, 2024The viral Artificial Intelligence trend has taken over social media, and artists...